Schwannomatosis are genetic syndromes predisposing to develop multiple schwannomas, and more rarely meningiomas1. These are rare diseases, with the most recent epidemiological data indicating a prevalence of 1 in 126,315 persons and an incidence of 1 in 68,956 births2.
Unlike patients with neurofibromatosis, patients with schwannomatosis often have non-specific symptoms, thus explaining the delay of several years between the appearance of the first symptoms and diagnosis. This delay is accentuated by the fact that familial forms, in which at least one of the parents is affected, are much rarer than sporadic forms in which neither parent is affected.
Within each of the two clinical forms (familial or sporadic), there is a subgroup of patients with so-called segmental schwannomatosis in which only one limb is affected.
Schwannomatosis are linked to germline mutations exclusive to each other in two tumour suppressor genes, SMARCB13 and LZTR1, both located on chromosome 22, as is the NF2 gene. SMARCB1 mutations are present in 40-45% of familial forms and 8-10% of sporadic forms. As for LZTR1 mutations, they are present in 30-35% of familial forms and 25-30% of sporadic forms.
Therefore, a large proportion of familial and sporadic schwannomatosis currently have no known genetic cause5. The formation of each schwannoma results from a 3-step mechanism of tumorigenesis:
- The first is the germline mutation of the tumour suppressor gene (SMARCB1 or LZTR1).
- Followed by somatic inactivation of the second allele of chromosome 22 by loss of heterozygosity.
- Then occurs a somatic mutation of the NF2 gene, resulting in bi-allelic inactivation of the 2 tumour suppressor genes.
Patients with schwannomatosis are classically diagnosed between 20 and 40 years of age, with the main symptoms at presentation being pain (46%), palpation of a mass (27%), or both (11%). Sensory-motor deficits are rare at presentation.
Patients mainly present with peripheral nerve schwannomas (89%) and spinal schwannomas (74%). Schwannomas of the cranial nerves are rare (8%): unilateral vestibular schwannoma can be found in 15% of patients with LZTR1-related schwannomatosis, and trigeminal schwannomas in other cases. Unilateral vestibular schwannomas, although rare, can be observed in patients with schwannomatosis.
Intracranial meningiomas are also rare (5%), present only in SMARCB1-related schwannomatosis and predominate at once6.
Schwannomatosis diagnosis is one of exclusion, the purpose of the initial assessment being to eliminate neurofibromatosis type 2. The initial imaging assessment thus includes a brain MRI with thin sections centred on the internal auditory canals, a pan-medullary MRI, and one or more MRI focused on the painful regions depending on each patient. If possible, whole-body imaging (MRI) or PET-MRI is recommended during the initial assessment of the disease.7 The diagnosis of schwannomatosis is a diagnosis of exclusion, the aim of the initial work-up being to eliminate neurofibromatosis type 2. The initial imaging work-up therefore includes a brain MRI with thin sections centred on the internal auditory canals, a pan-medullary MRI and one or more MRIs centred on the painful regions depending on the patient. If possible, whole-body imaging (MRI or PET-MRI) is recommended as part of the initial examination of the disease.
The MRI follow-up is then annual and focuses on the painful areas. The schwannomas of patients with schwannomatosis have the same radiological appearance as sporadic schwannomas, except for multi-nodular forms, which result from the fusion of multiple contiguous schwannomas on the same peripheral nerve. High-resolution MRI neurography can also reveal multiple intrafascicular micro lesions along peripheral nerves8. These micro lesions are also found in all limbs of patients with segmental schwannomatosis, in which macroscopic schwannomas and pain are limited to a single limb. There is therefore no definite link between these micro-nerve lesions and patients' pain. Electrophysiological assessments are also often normal in patients with schwannomatosis.9.
The management of patients with schwannomatosis is carried out in a "rare diseases" centre that combines clinical management with genetic diagnosis and counselling. On the clinical side, the management of patients with schwannomatosis is focused on the treatment of chronic pain, which is present in 68% of patients. This pain is often poorly localised, presenting by access on a permanent painful background, and often unrelated to an underlying schwannoma6. The treatment is therefore essentially medical, with many cases of rebellious pain: 27% of patients report the use of more than six painkillers6.
Surgery remains indicated for cases of rapidly growing tumours or explicitly causing the symptoms. Surgery for peripheral schwannomas in schwannomatosis is accompanied by a slightly lower rate of pain relief than that in the sporadic forms (74.5%). Surgery is also accompanied by a higher number of post-operative deficits in patients with schwannomatosis, around 25%. These deficits predominate in patients with multi-segmental forms with the removal of multiple tumours during the same procedure or the removal of tumours in a string on the same nerve10. The effects of radiotherapy and chemotherapy in the treatment of schwannomatosis are, so far, very limited.
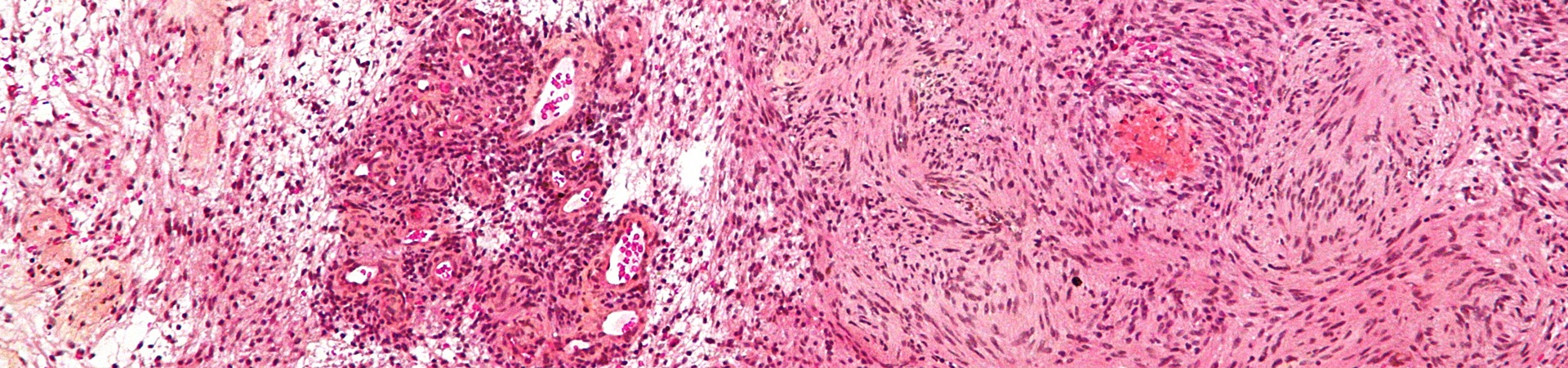
The natural history of the disease is marked by the discovery of new schwannomas during the disease follow up10, 11, although it is not clear whether this finding is related to the incompleteness of the initial workup, which rarely includes a whole-body MRI at present, or to an evolution of the tumour load over time. Cases of malignant transformation of peripheral schwannomas have been reported in schwannomatosis10, mainly in SMARCB1 related forms, but their reality remains uncertain so far as all the reported cases of malignant transformations in the reference series have been checked after neuropathological expertise6.
Michel Kalamarides
Referral centre for neurofibromatosis type 2 and schwannomatosis
AP-HP - Pitié-Salpêtrière Hospital - 75013 - Paris - France
Matthieu Peyre
Sorbonne University – Neurosurgery department
AP-HP – Pitié-Salpêtrière Hospital – 75013 – Paris – France
- MacCollin M, Woodfin W, Kronn D, Short MP. Schwannomatosis: a clinical and pathologic study. Neurology. 1996 Apr;46(4):1072–9.
- Evans DG, Bowers NL, Tobi S, Hartley C, Wallace AJ, King AT, et al. Schwannomatosis: a genetic and epidemiological study. J Neurol Neurosurg Psychiatry. 2018 Jun 16;
- Hulsebos TJM, Plomp AS, Wolterman RA, Robanus-Maandag EC, Baas F, Wesseling P. Germline mutation of INI1/SMARCB1 in familial schwannomatosis. Am J Hum Genet. 2007 Apr;80(4):805–10.
- Piotrowski A, Xie J, Liu YF, Poplawski AB, Gomes AR, Madanecki P, et al. Germline loss-of-function mutations in LZTR1 predispose to an inherited disorder of multiple schwannomas. Nat Genet. 2014 Feb;46(2):182–7.
- Hutter S, Piro RM, Reuss DE, Hovestadt V, Sahm F, Farschtschi S, et al. Whole exome sequencing reveals that the majority of schwannomatosis cases remain unexplained after excluding SMARCB1 and LZTR1 germline variants. Acta Neuropathol (Berl). 2014 Sep;128(3):449–52.
- Merker VL, Esparza S, Smith MJ, Stemmer-Rachamimov A, Plotkin SR. Clinical features of schwannomatosis: a retrospective analysis of 87 patients. The Oncologist. 2012;17(10):1317–22.
- Ahlawat S, Fayad LM, Khan MS, Bredella MA, Harris GJ, Evans DG, et al. Current whole-body MRI applications in the neurofibromatoses: NF1, NF2, and schwannomatosis. Neurology. 2016 Aug 16;87(7 Suppl 1):S31-39.
- Farschtschi S, Mautner V-F, Pham M, Nguyen R, Kehrer-Sawatzki H, Hutter S, et al. Multifocal nerve lesions and LZTR1 germline mutations in segmental schwannomatosis. Ann Neurol. 2016 Oct;80(4):625–8.
- Schulz A, Grafe P, Hagel C, Bäumer P, Morrison H, Mautner V-F, et al. Neuropathies in the setting of Neurofibromatosis tumor syndromes: Complexities and opportunities. Exp Neurol. 2018;299(Pt B):334–44.
- Gonzalvo A, Fowler A, Cook RJ, Little NS, Wheeler H, McDonald KL, et al. Schwannomatosis, sporadic schwannomatosis, and familial schwannomatosis: a surgical series with long-term follow-up. Clinical article. J Neurosurg. 2011 Mar;114(3):756–62.
- El Sayed L, Masmejean EH, Parfait B, Kalamarides M, Biau D, Peyre M. Natural history of peripheral nerve schwannomas. Acta Neurochir (Wien). 2020 Aug;162(8):1883-1889.